Raised PSA
We offer a range of tests and diagnostics to identify the cause of raised PSA before recommending the best course of treatment for your individual case.
PSA (prostate-specific antigen) Test
One in eight men in the UK will get prostate cancer. The good news is that early diagnosis and treatment can lead to much better patient outcomes.
A PSA test is a simple means of early identification of problems with the prostate, including prostate cancer. The test itself is very simple and involves taking a sample of blood which is then tested to identify the level of PSA present. Prostate-specific antigen (PSA) is a small protein that is secreted from the prostate into the blood and is measured in the blood in nanograms per millilitre (ng/mL).
It’s perfectly normal for men to have a small amount of PSA in their blood. However, the prostate can enlarge for several reasons, resulting in elevated levels of PSA.
These reasons include:
- Benign prostate enlargement
- Inflammation as a result prostatitis
- Urinary infection
- Prostate cancer
Who should have a PSA test?
Because men’s prostates tend to enlarge with age, it’s not unusual for levels of PSA in the blood to increase as they get older.
It is therefore advisable for men who meet any of the following criteria to know what their normal PSA level is. And then test regularly to identify any changes from the norm.
- Men aged 50 and over.
- Men aged 45 and over at higher risk of prostate cancer:
- have a family history of prostate cancer or breast cancer
- are of black ethnic origin
- are overweight or obese
- Men with symptoms of a potential prostate problem such as needing to urinate more frequently, more urgently or experiencing problems with emptying the bladder.
Should their PSA level persistently fall above the normal level for their age, then a consultant urologist would be keen to pursue further diagnostic tests.
At the Urology Partnership we conduct a digital rectal examination (DRE) alongside a PSA test.
Digital rectal examination (DRE) or per-rectal examinations (PR)
The back of the prostate (posterior aspect) lies next to the lining of the rectum and can be easily felt when a trained professional inserts a lubricated gloved finger into the rectum to feel the shape and texture of the prostate glands.
Although it is a somewhat undignified procedure to undergo, it is completely painless. It does not in itself completely exclude prostate cancer but taken together with a PSA blood test is very valuable to a consultant urologist.
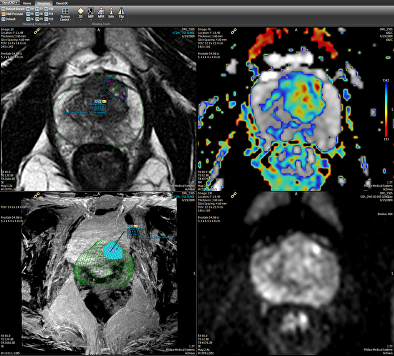
If an elevated PSA blood test plus / minus an abnormal feeling prostate is found, then the next stage of an investigation is a multi-parametric MRI scan of the prostate.
Raised PSA FAQs
The following video provides an overview of the role of the prostate and symptoms to look out for that could indicate a prostate problem.
Please look at these links for further information on raised PSA and prostate cancer:
Next Steps
Our Raised PSA Specialists
Get fast access to leading specialists for the swift diagnosis and treatment of urological conditions in a private clinic environment.
If you would like more information or wish to arrange a consultation with one of our specialist consultant urological surgeons then please either Call 0118 920 7040 or complete the form below.
Insured patients
Contact your GP and ask for a referral to the Urology Partnership.
All consultations, investigations and treatments are covered by major insurance companies (depending on policy).
Funding your own treatment
Self-funding initial consultation fee is £205. Follow up fees are £165.
Consultation charges are exclusive of any tests and other investigations that the consultant may wish to carry out.




