Prostatitis
Chronic prostatitis / chronic pelvic pain is becoming an increasing problem, and can lead to miserable symptoms that can severely affect the quality of a man’s life.
Overview of Prostatitis
Male urinary tract infections (UTIs), also commonly referred to as ‘prostatitis’, is an increasing problem worldwide and is often difficult to treat or eradicate.
Part of the problem is that infections in men can become deep seated within the prostate, which is termed ‘chronic bacterial prostatitis’. This can lead to miserable symptoms that can severely affect the quality of a man’s life.
Furthermore the body’s own response to fighting an infection can lead to long lasting inflammation within the prostate, known as ‘inflammatory prostatitis’ or ‘inflammatory chronic pelvic pain syndrome’.
For many years there has been little that can be done for men with this very debilitating condition, however the specialist consultants at The Urology Partnership have established the latest diagnostic and treatment options in a dedicated clinic for men with this condition.
What is the most common cause of prostatitis?
Our consultant urologist, Mr Chris Blick, talks about the most common cause of prostatitis and then talks about bacterial prostatitis and how that can be treated.
Symptoms of Prostatitis
- Pain in and around your penis, testicles, anus, lower abdomen, or lower back
- Pain when peeing, a frequent or urgent need to pee, particularly at night, or “stop-start” peeing
- An enlarged or tender prostate on rectal examination, although in some cases it may be normal
- Sexual problems, such as erectile dysfunction, pain when ejaculating, or pelvic pain after sex
Diagnosing Prostatitis
Multiple investigations are often needed to get a clear diagnosis of the cause of chronic prostatitis / chronic pelvic pain, and to exclude any serious underlying pathology or cancer.
The investigations below can often be performed on the same day as the initial consultation (depending upon insurance company criteria):
- Consultant Surgeon initial meeting and examination
- Urinary flow assessment & post micturition bladder volume scan assessment
- Urine analysis and urine microscopy and culture
- Blood tests (incl. PSA, PCA)
- Urine Cytology / NMP 22
- Ultrasound scanning by consultant uro-radiologist
- Flexible cystoscopy
- Urodynamic bladder studies
- Multiparametric MRI of the prostate (separate day – currently performed at Spire Dunedin Hospital).
The other differential diagnosis that needs to be considered is if symptoms of prostatitis (whether infective or inflammatory) are mimicking a more serious underlying pathology, such as cancer, or whether the pain / symptoms are referred from other neuromuscluar causes, such as pudendal nerve irritation.
Treatments for Prostatitis
Treatments for prostatitis include:
1. Antibiotics
2. Intra-vesical treatments
3. Radio frequency pulse heat treatment to pudendal nerve
1. Antibiotic Treatment
The standard treatment is with antibiotics which most patients with a single episode respond to very well.
Our approach to the selection of antibiotics is tailored to the individual patient based on unique sensitivity profiling of urine cultures and clinical judgement of best antibiotic according to it’s specific bio-availability. In men this is particularly important to ensure the best penetration of antibiotic into the prostate and its secretions.
Once the infections become more chronic, antibiotic treatments range from keeping antibiotics at home, to going onto a low dose antibiotic where you take one every night or just one antibiotic after sexual intercourse.
There is currently a lot of concern about long-term use of antibiotics and although they are well recognised and well established, alternative treatments are becoming more popular.
2. Intra-vesical Treatments
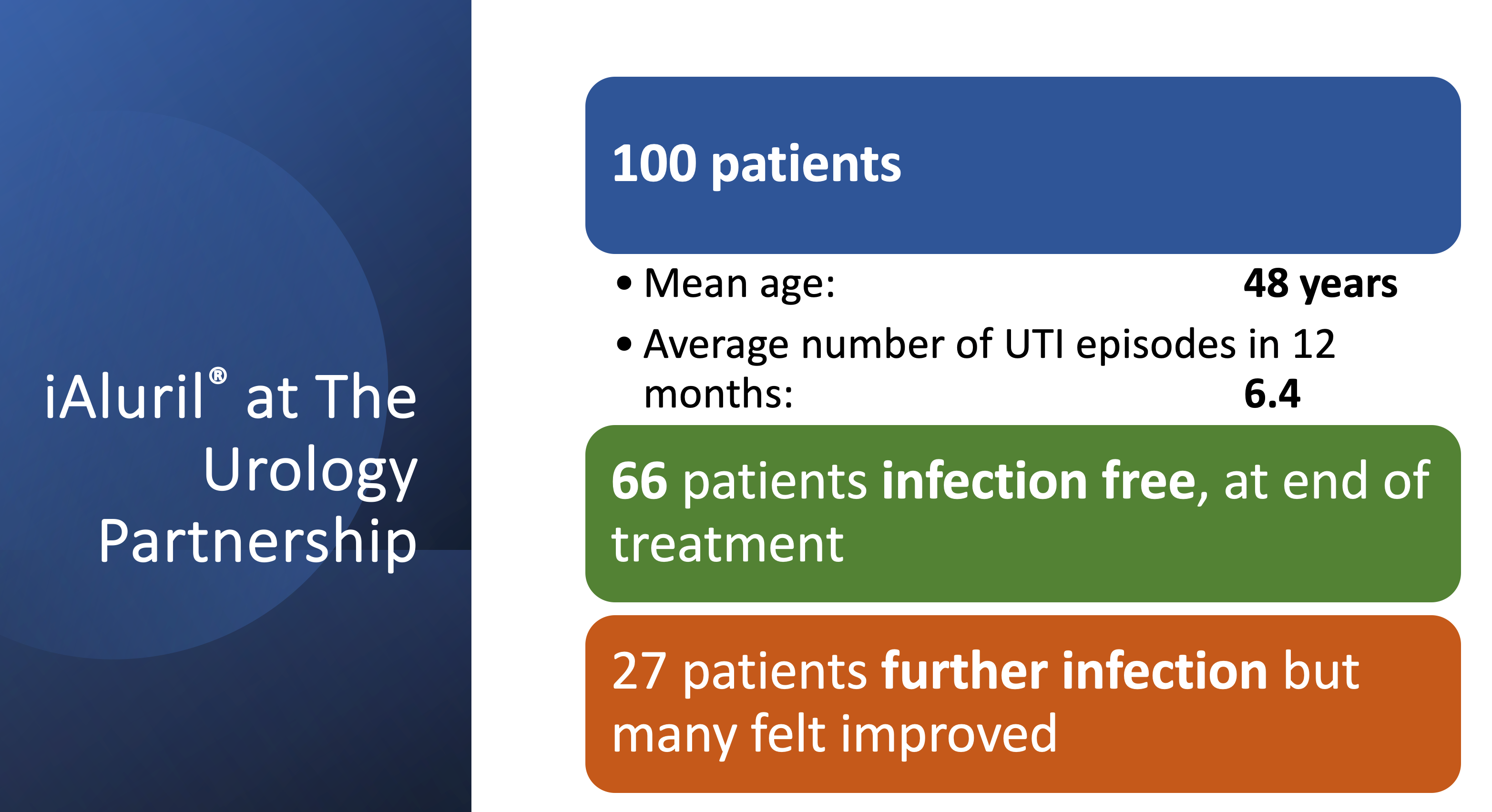
Part of the problem with patients with recurrent urinary tract infections is a deficiency in the lining of the bladder which makes them much more susceptible to infections with low levels of bacteria. A well established treatment now, is a course of bladder installations which can be performed either by the nurse or by the patient themselves once a week for six weeks, followed by a monthly course for six months. These are available in many NHS hospitals, covered by insurance companies and are very well tolerated.
Seventy percent of patients with recurrent infections respond well to intra-vesical treatments with both an increase in bladder comfort and a reduction in infection rates.
3. Non-inflammatory Prostatitis
In the same way as lower back problems can irritate the sciatic nerve causing pain that radiates down the outside of the leg (in the distribution of the sciatic nerve), the pudendal nerve, or its nerve roots can become irritated. This can cause pain and dysfunction of the areas and organs it supplies, including the penis, the perineum and the bladder. Exclusion of other causes together with MRI scanning of the pelvis and lower spine can point towards this often overlooked cause of chronic pelvic pain syndrome.
There are numerous treatment options that can be very helpful for this problem, including specialist physiotherapy, nerve modulating medications, epidural / spinal injections as well as nerve root radiofrequency heat treatment.
Next Steps
Get fast access to leading specialists for the swift diagnosis and treatment of urological conditions in a private clinic environment.
If you would like more information or wish to arrange a consultation with one of our specialist consultant urological surgeons then please either Call 0118 920 7040 or complete the form below.
Insured patients
Contact your GP and ask for a referral to the Urology Partnership.
All consultations, investigations and treatments are covered by major insurance companies (depending on policy).
Funding your own treatment
Self-funding initial consultation fee is £205. Follow up fees are £165.
Consultation charges are exclusive of any tests and other investigations that the consultant may wish to carry out.
